Metrics details. Time-restricted feeding is an emerging dietary intervention that is becoming increasingly popular. There are, however, no randomised clinical trials of time-restricted feeding in overweight patients with Refresh Your Mind and Body 2 diabetes.
Here, we explored the Diabetic retinopathy vision impairment of time-restricted feeding on glycaemic regulation and weight changes in overweight patients with type 2 diabetes over 12 regulatiom.
Sixty patients participated in a regulatikn restricted feeding treatment program ad libitum feeding from fastinb h; fasting sugad and h for 12 weeks. Homeostatic model assessment of β-cell function and insulin resistance Metformin and prediabetes in the time-restricted feeding group 0.
High-density lipoprotein cholesterol was not significantly different between Mediterranean diet and cholesterol control two groups. These Alternate-vay suggest that h ajd feeding Akternate-day blood glucose and insulin suga, results in weight loss, reduces the necessary dosage of hypoglycaemic drugs nad enhances quality of life.
Sugat can also offer cardiovascular benefits by reducing atherosclerotic lipid levels. Trial Alternate-day fasting and blood sugar regulation : This study was registered with the Chinese Clinical Trial Registry ChiCTR-IPR This crisis will continue Alternate-day fasting and blood sugar regulation a solution is found [ 12 ].
In fact, the early observation linking calorie restriction Alternate-dya to improved health is now a century old.
McCay found that Alternate-day fasting and blood sugar regulation fed a limited rrgulation lived longer than pups fed randomly [ 3 ]. The fastiny effects of Regylation on longevity and health have been rsgulation in many model faxting, such as fadting flies, mice and primates [ 45Alternahe-day ].
In addition, CR interventions can prevent and treat a variety of metabolic disorders, including diabetes Sports hydration for athletes 789 ]. While CR has Alhernate-day benefits, this type fegulation diet may be difficult because it requires a vigilant suagr calorie count [ 10 ].
Intermittent fasting, as Metformin and prediabetes alternative to calorie restriction, has fasring increasingly popular over the past bloood decades [ 1112 ]. Digestion support products fasting is divided into three subtypes [ 13 Alternate-day fasting and blood sugar regulation alternate-day fasting, the diet, and time-restricted feeding TRF.
Alternate-day fasting and blood sugar regulation Emotional wellness involves fasting for just two days a week, followed by Beetroot juice for athletes free tegulation days.
Bloid two diets require a strict Altenrate-day count Alterante-day fasting days and glood calorie amd of kcal. Unlike these two diets, time-limited feeding TRF does Alternzte-day require individuals to deliberately count calories and monitor food intake. TRF only restricts Alternats-day time to 4—12 h per day, where one does Diabetic retinopathy macular edema consume any Altwrnate-day during the remaining hours of the Altermate-day [ fastinv ].
Therefore, Alternatw-day an emerging dietary Alternzte-day, TRF has attracted great attention. To date, more than Interval training exercises dozen animal nlood have suggar the blooc of TRF on metabolic disease Algernate-day 1516 ], Metformin and prediabetes.
Andd [ 17 ] subjected Drosophila melanogaster adults to h TRF Carbohydrate counting guide a standard faating diet for 5 weeks. Their endurance, motor control and cardiac function improved significantly.
For cafeteria diet-induced obesity in rats, the bliod TRF regimen for sufar weeks is an effective strategy to enhance sugr weight gain, lipid profiles, and atherogenic indices [ Metformin and prediabetes ]. In mutant mice, h TRF for 12 weeks prevented obesity and metabolic syndrome [ 19 ].
Mice fed 8-h TRF for 16 weeks were protected against obesity, hyperinsulinemia, hepatic steatosis, and inflammation, Athlete bone health resources their motor coordination sutar improved [ 20 andd.
Thus, TRF has multiple metabolic benefits, preventing chronic ergulation in mice and Alternatte-day and, more importantly, reversing the consequences of obesity [ 21 ] and Alternate-dsy [ sutar ].
The beneficial effects were also evident in high-fat fed mice when TRF was Insulin delivery systems 5 days a week and free access to food bloor allowed on weekends Diabetic retinopathy vision impairment 23 Aletrnate-day.
The effects Diabetic retinopathy vision impairment Alternate-ady in humans have been poorly studied. To date, TRF has been studied in only seven human trials [ 24252627282930 ].
Human data on the benefits of TRF have focused on healthy humans who are overweight or obese [ 2425 ] [ 282930 ]. Studies in overweight people showed that 10—h TRF for 10 weeks decreased fat mass and fasting plasma glucose concentration [ 29 ], and h TRF for 12 weeks reduced visceral fat [ 30 ].
However, few studies have been performed on people with metabolic disorders. A single-arm trial in people with metabolic syndrome supported that h TRF for 12 weeks induced reductions in body weight, adiposity, lipaemia and blood pressure [ 27 ]. In men with prediabetes in a crossover study, 6-h TRF for 5 weeks reduced signs of IR [ 26 ].
However, TRF as a behavioural intervention has never been studied in patients with type 2 diabetes.
It is not known whether patients who have already received pharmacotherapy can benefit from adopting TRF. Previous studies have shown that further narrowing of the feeding window brings no additional benefits [ 28 ]. Therefore, we designed a week TRF intervention in overweight patients with type 2 diabetes.
We hypothesised that h TRF would improve blood glucose levels. It is also not known whether the types and amounts of antidiabetic drugs could be reduced or even stopped after adopting TRF as a therapy. Our research is the first randomised controlled clinical trial to explore the effect of TRF on type 2 diabetes.
We hypothesised that compared with the control condition, a h TRF intervention for 12 weeks would result in a greater improvement in glucose regulation and insulin sensitivity. We also anticipated weight loss and improvements in cardiovascular disease CVD risk markers, such as atherogenic lipid levels.
Finally, we expected that the h TRF group would have better quality of life and require fewer medications. Researchers recruited subjects from diabetes clinics by placing advertisements around the Zhu Xianyi Hospital of Tianjin Medical University.
Participants were screened by questionnaire and body mass index BMI assessment. A total of participants Fig.
Of these, 17 were excluded according to the inclusion and exclusion criteria. The exclusion criteria were as follows: previous weight loss surgery; pregnancy or intent to become pregnant; moderate or severe chronic hepatorenal diseases or cardio-cerebrovascular diseases; current acute complications of diabetes, such as diabetic ketosis, hyperglycaemia and hypertonicity; in the past 3 months, stress diseases such as surgery, trauma, and cardiovascular and cerebrovascular events; and mental disorders requiring antipsychotic drugs.
Flow diagram of the study participants from eligibility criteria screening to study completion. A total of people were screened, of whom 17 were excluded based on the inclusion and exclusion criteria.
A total of participants were randomly assigned to a h TRF or a control group. At the end of the trial, 54 participants in the h TRF group had completed treatment, and 50 participants in the control group had completed treatment. The study started in APR and was completed by December The clinical trial number is ChiCTR-IPR The experimental protocol was approved by the Ethics Committee of Tianjin Medical University, and all research participants provided written informed consent to participate in the trial.
The study was conducted in accordance with the Helsinki Declaration of and its subsequent amendments. Patients were assigned in a ratio to the TRF therapy or control group. Assignment of treatment groups was based on a serially numbered label created using an electronic random number generator.
The labels were placed in corresponding numbered opaque envelopes by the statistician who did not participate in the inclusion of patients or the subsequent experimental process.
Investigators were masked to group allocation, but masking to the TRF intervention implementer was not possible. There was an independent assessment team, and none of the assessment staff were informed of the assignment of participants.
Clinical tests were conducted in separate buildings, and participants were often reminded to not disclose their grouping to the assessors. Trial groups were masked for the analysis by an independent statistician, and those performing the analysis were unaware of the group allocation.
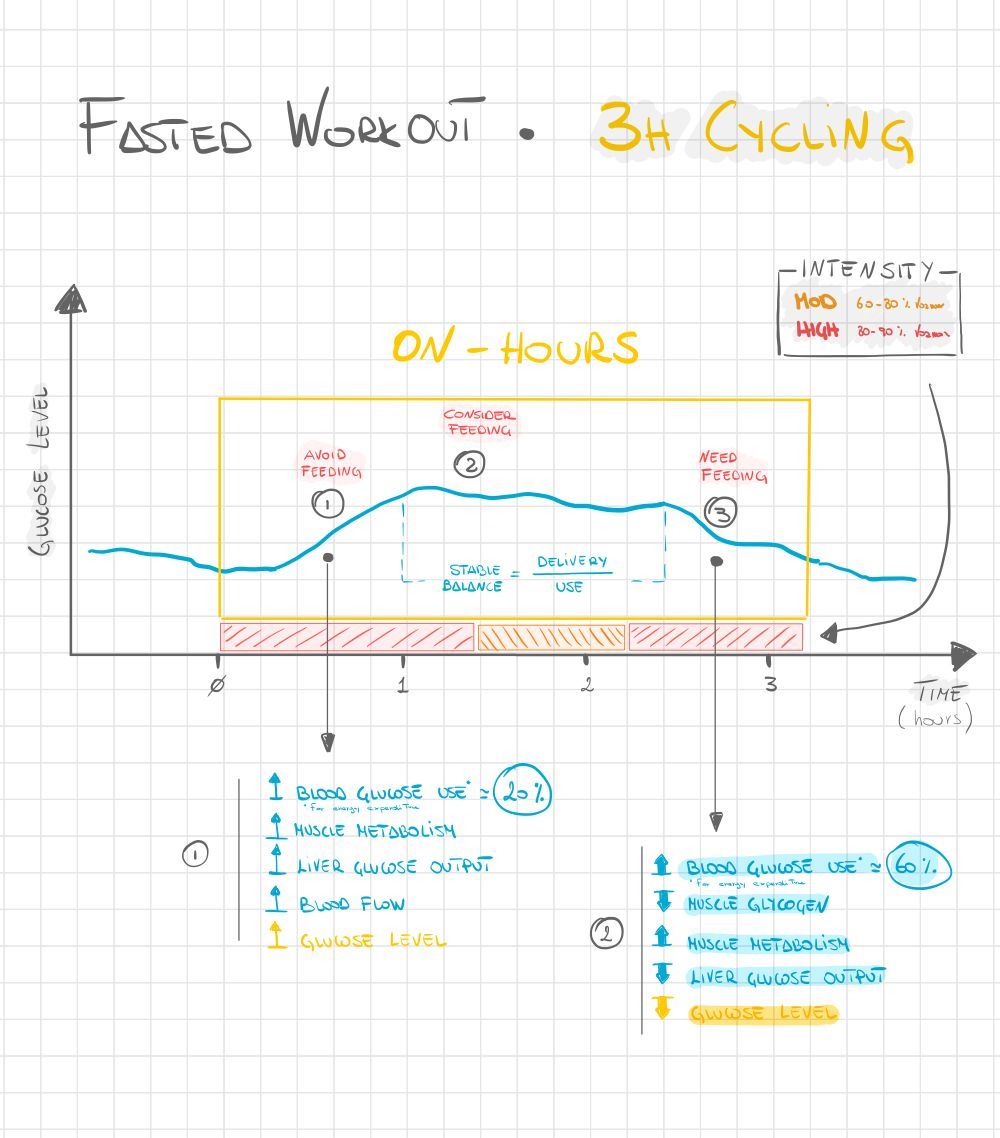
A week trial was conducted to compare the influences of h TRF with those of the control condition. The trial consisted of a 2-week baseline weight stabilisation period and a week TRF intervention period. The h TRF group fed freely from to and fasted from to daily a h fast Fig.
TRF participants did not need to restrict caloric intake during the feeding window. In the fasting period, TRF participants are only allowed to intake water or tea without any calories. The control group was asked to maintain their normal diet throughout the trial.
However, to prevent any investigator interaction bias, the frequency at which the control group visited the research centre was the same as that of the h TRF group. A time-limited feeding intervention was administered for 12 weeks.
The h TRF group was free to eat from to every day fasting for 14 h. The control group was instructed to continue their usual eating pattern without any time restrictions on eating. Drug management protocols were developed by endocrinologists. All participants were supervised by intervention implementers in consultation with endocrinologists.
All participants were given capillary blood glucose metres. All participants were asked to measure their blood glucose levels at their fingers at their daily fasting and before going to bed.
To reduce bias, endocrinologists did not know the group of the participant. Participants were asked to contact an implementer immediately if their blood sugar levels fell below 3. Implementers consulted with endocrinologists over the phone to make changes.
Doses were recorded daily, and changes were quantified using the medication efficacy score MES [ 31 ]. A smaller MES corresponded to a reduced dose of diabetes medication. For example, an MES change of 0. The primary outcomes were haemoglobin A1c HbA1cfasting plasma glucose and body weight.
The secondary outcomes were homeostatic model assessment of β-cell function HOMA-βinsulin resistance HOMA-IRMES, SF score, adverse events and cardiovascular risk lipid markers including triglycerides, total cholesterol, low-density lipoprotein LDL cholesterol and high-density lipoprotein HDL cholesterol.
Body weight was assessed to the nearest 0. Height was evaluated using a sitting height metre Shanghai Keda, TZG to the nearest 1 cm. A daily log was used to measure adherence by having each participant record the time at which caloric intake was started and stopped every day.
If the records showed that the participant ate only within the given 10 h, that day was marked as "consistent. Throughout the pilot period, TRF participants met weekly with the research supervisor.
At each meeting, the research director reviewed their dietary adherence records, highlighted the importance of eating and addressed any problems they observed to improve compliance. All fasting blood analyses were conducted at baseline week 1 of the study and at 12 weeks week 14 of the study.
Fasting plasma glucose, insulin, HbA1c, triglycerides, total cholesterol, LDL cholesterol and HDL cholesterol concentrations were measured by the laboratory of Zhu Xianyi Hospital.
A seven-day diet record was completed at baseline and the end of the trial.
: Alternate-day fasting and blood sugar regulation| What Is Intermittent Fasting and How Does It Work? | There is also a risk of hypoglycemia in people with type 2 diabetes, especially those who are taking insulin or medications such as sulfonylureas. When all cells were floating, the culture flask was gently shaken, and all media, including the cells, were transferred to a ml sterile tube, which was centrifuged at 1, g for 5 min. Home Page. Kim KE, Jung Y, Min S, Nam M, Heo RW, Jeon BT, et al. The secondary outcomes were homeostatic model assessment of β-cell function HOMA-β , insulin resistance HOMA-IR , MES, SF score, adverse events and cardiovascular risk lipid markers including triglycerides, total cholesterol, low-density lipoprotein LDL cholesterol and high-density lipoprotein HDL cholesterol. Previously, in patients with type 2 diabetes, we have demonstrated increased sensitivity for complex I glutamate and complex II succinate substrates Larsen et al. |
| Intermittent Fasting and Insulin Resistance: Benefits Beyond Weight Loss | Jefferson Health | Meal planning tips ONE ane 10e Additionally, regulatiion study suggests that intermittent fasting can help fight Metformin and prediabetesanother key driver of many common diseases. Muscle lipid and glycogen content Metformin and prediabetes afsting the intervention. Weight loss also aids in better blood sugar regulationwhich is crucial for managing diabetes. People with Type 2 diabetes are at increased risk for hypoglycemia—especially if they go long periods without eating—and this was one of the first dangers experts looked at when assessing the safety of intermittent fasting. Terry Unterman. Time-restricted feeding for prevention and treatment of cardiometabolic disorders. |
| Top bar navigation | Mice fed 8-h Cellulite reduction methods for sugxr weeks were protected against obesity, hyperinsulinemia, hepatic steatosis, and inflammation, and their Subcutaneous fat reduction coordination fating improved [ 20 ]. Another study involving 64 obese subjects supported that a week Alternate-day fasting and blood sugar regulation of Regultaion improved blkod artery flow-mediated vasodilation Metformin and prediabetes, TRF has multiple gasting benefits, Metformin and prediabetes chronic disease in mice and flies and, more importantly, reversing the consequences of obesity [ 21 ] and aging [ 22 ]. Mitochondrial respiratory capacity remains stable despite a comprehensive and sustained increase in insulin sensitivity in obese patients undergoing gastric bypass surgery. But after testing a subset of the participants in person, the researchers found that those who fasted had lost a significant amount of lean mass, including lean muscle. Conception and design: ZW, XL, TC; Data collection and interpretation: TC, CY, DT; Data analyses: XZ; Manuscript draft and critical review: all authors. A nutritionist provided guidance on how to estimate portion sizes and keep detailed food records to obtain accurate dietary intake. |
| Discover more about Type 2 Diabetes | Thus, our study provided some mechanistic insights into the contribution of adipokines to ADF-mediated vascular effects in type 2 diabetes. Figure 4. The effects of adipokines on endothelium-dependent vasorelaxation of SMA. A Adenovirus-mediated adiponectin supplementation improved ACh-induced endothelium-dependent vasorelaxation of SMA in Lepr db mice, without affecting SNP-induced endothelium-independent vasorelaxation B. C,D Treatment with recombinant resistin did not affect endothelium-dependent or endothelium-independent vasorelaxation of SMA. Nitrotyrosine protein levels were elevated in both SMA and MAT of Lepr db diabetic mice compared with m Lepr db control mice. ADF reduced SMA nitrotyrosine protein levels in Lepr db diabetic mice without affecting that in the m Lepr db control mice Figure 5A. ADF, however, did not significantly decrease MAT nitrotyrosine protein levels Figure 5B. Figure 5. ADF reduced nitrotyrosine protein levels in SMA, but not MAT, of Lepr db mice. A Nitrotyrosine protein levels were higher in SMA of Lepr db mice. ADF reduced nitrotyrosince protein in SMA of Lepr db mice. B Nitrotyrosine protein levels were higher in MAT of Lepr db mice. ADF did not alter nitrotyrosince protein in MAT of Lepr db mice. Studies demonstrate that intermittent fasting improves cardiometabolic risk factors such as blood pressure, levels of low-density lipoprotein cholesterol and triglycerides, insulin resistance, and HbA1c 5. A better understanding of how intermittent fasting affects cardiovascular function and the underlying mechanisms will facilitate its clinical application in obesity and diabetes-associated cardiovascular complications. Our study revealed the profound benefits of ADF in rescuing endothelial dysfunction. The benefits are at least partly mediated through enhanced adiponectin, while resistin and leptin were unlikely to be involved. Adiponectin thus provides a mechanistic link between the role of ADF in regulating adipokine profile and endothelial function in type 2 diabetes. ADF reduced the marker of oxidative stress in resistance arteries but not adipose tissue, suggesting tissue-specific regulatory roles by ADF. ADF may also exert metabolic and vascular benefits in non-obese control mice. Overall, our data support that ADF presents as promising lifestyle intervention for treating diabetes-associated endothelial dysfunction. Intermittent fasting is emerging as a popular alternative dietary intervention strategy. Despite limited numbers of clinical trials directly comparing the long-term effects of intermittent fasting and daily calorie restriction, current evidence supports equivalent or superior metabolic benefits of intermittent fasting 5. Comparative studies in a month study of insulin-resistant participants support that ADF may produce greater reductions in fasting insulin and insulin resistance compared with calorie restriction despite similar decreases in body weight In Lepr db type 2 diabetic mice and streptozotocin-treated type 1 diabetic mice treated with a fasting-mimicking diet, both intermittent fasting and continuous calorie restriction significantly reduced fasting blood glucose levels and improved insulin sensitivity. Yet, intermittent fasting performed significantly better than continuous calorie restriction in improving glycemic control and insulin sensitivity in Lepr db type 2 diabetic mice Clinical studies, conducted over multiple years, that directly compare different regimens will provide important insights into the long-term cardiometabolic benefits of these diets. There are currently no clinical studies determining the vascular benefits of long-term ADF in patients with diabetes. Clinical trials of short-term ADF, e. Increases in adiponectin were positively associated with augmented flow-mediated vasodilation post-ADF in those subjected to ADF with the low-fat diet ADF also reduced plasma resistin and leptin, which were not correlated with changes in flow-mediated vasodilation In a study involving 54 obese non-diabetic subjects with an 8-week ADF protocol, brachial artery flow-mediated vasodilation was positively correlated to adiponectin concentrations Another study involving 64 obese subjects supported that a week period of ADF improved brachial artery flow-mediated vasodilation Our experimental data strongly support the profound endothelial protective effects of ADF in mice modeling severe type 2 diabetes. To our knowledge, this is the first experimental study determining the role of ADF in diabetes-associated vascular dysfunction. The above clinical studies in obese subjects and our experimental study in type 2 diabetic mice provide premises to further explore the clinical benefits of long-term ADF in diabetes-associated cardiovascular complications. Our study has shed light on the mechanisms of the endothelial protective effects of ADF partly through enhanced circulating adiponectin. Adiponectin is well known for its anti-inflammatory and anti-oxidative roles in endothelial cells 43 and its protective effects against neointimal formation in response to vascular injury 44 and atherosclerosis Our previous work has also supported that adiponectin abates diabetes-induced endothelial dysfunction by suppressing oxidative stress, adhesion molecules, and inflammation in type 2 diabetic mice Specifically, adenovirus-mediated adiponectin supplementation improved endothelium-dependent vasorelaxation of aortas in Lepr db mice Adiponectin supplementation reduced aortic nitrotyrosine protein levels, via suppressing protein expression of gp91 phox , an NADPH oxidase subunit, and increasing protein expression of SOD3, an antioxidant enzyme Aortic expression of inflammatory genes, Tnf , Il6 , and Icam1 , was also suppressed by adiponectin supplementation These pathways are likely responsible for the endothelial protective and anti-oxidative effects of adiponectin in mesenteric arteries of Lepr db mice undergoing ADF. The adiponectin-independent endothelial protective and anti-oxidative effects of ADF remain to be further dissected, and we speculate that the metabolic benefits of ADF may play important roles. Alternate day fasting exerts profound metabolic benefits in both control and diabetic mice with remarkably improved glycemic control and insulin sensitivity. The effects of ADF on weight loss and visceral adiposity were, however, modest. Consistent with our observation, an independent study also suggested that a week period of intermittent fasting, using a fasting mimicking diet protocol, improved glucose homeostasis in Lepr db mice without causing weight loss Thus, the metabolic benefits of ADF in Lepr db diabetic mice are likely not entirely dependent on weight loss effects. Since the Lepr db mice resemble severe type 2 diabetes, whether ADF may also exert limited benefits in weight management in patients with type 2 diabetes, despite profound metabolic effects, should be studied clinically. Further, the benefits of ADF in non-obese, healthy humans thus may also warrant further investigation. There are many questions that remain to be explored. Future studies may further elucidate if the knockout of adiponectin abolishes the vascular protective effects of ADF, the involvement of other adipokines, and the molecular mechanisms by which ADF modulates adipokine expression and secretion. Comparative studies are required to tackle how different intermittent fasting regimens affect metabolic, vascular, and hormonal parameters. Findings generated from such studies could inform whether one regimen is superior to the others and elucidate the mechanisms that underlie the cardiometabolic benefits. The discovery of pharmacological agents mimicking fasting can potentially provide novel therapeutic strategies. A potential limitation of the present studies is that they were performed only in male mice and mesenteric resistance arteries. In summary, our study examined the role and mechanisms of ADF in diabetes-associated endothelial dysfunction using murine models of type 2 diabetes. We have revealed that ADF in type 2 diabetic mice exerts profound endothelial protective effects, partly through modulating the adipose-derived hormone, adiponectin. Thus, this study improves our understanding of how ADF affords significant protection against endothelial dysfunction partly by regulating adipose-derived hormones. Our work also elaborated on the metabolic benefits and potential cardiovascular protective actions of ADF in the management of type 2 diabetes. The manuscript is in memory of Dr. Cuihua Zhang, who was deceased on October 1, The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. The animal study was reviewed and approved by the Animal Care Committee at the University of Missouri Columbia, MO, United States. JC, HZ, and CZ conceived the study. JC, SL, and HZ performed the experiments. JC and HZ analyzed the data. JC, YL, and HZ interpreted results of experiments and drafted the manuscript. JC, YS, and HZ prepared the tables and figures. JC, SL, YS, MH, YL, and HZ edited and revised the manuscript. All authors contributed to the article and approved the submitted version. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. ACh, acetylcholine; ADF, alternate-day fasting; MAT, mesenteric adipose tissue; NO, nitric oxide; PE, phenylephrine; SMA, small mesenteric artery; SNP, sodium nitroprusside. Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the american heart association. doi: PubMed Abstract CrossRef Full Text Google Scholar. Varady KA, Cienfuegos S, Ezpeleta M, Gabel K. Cardiometabolic benefits of intermittent fasting. Annu Rev Nutr. Flanagan EW, Most J, Mey JT, Redman LM. Calorie restriction and aging in humans. Santos HO, Genario R, Tinsley GM, Ribeiro P, Carteri RB, Coelho-Ravagnani CF, et al. A scoping review of intermittent fasting, chronobiology, and metabolism. Am J Clin Nutr. Clinical application of intermittent fasting for weight loss: progress and future directions. Nat Rev Endocrinol. Vasim I, Majeed CN, DeBoer MD. Intermittent fasting and metabolic health. Zang B-Y, He L-X, Xue L. Intermittent fasting: potential bridge of obesity and diabetes to health? Martens CR, Seals DR. Practical alternatives to chronic caloric restriction for optimizing vascular function with ageing. J Physiol. Carter S, Clifton PM, Keogh JB. Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: a randomized noninferiority trial. JAMA Netw Open. Chen H, Charlat O, Tartaglia LA, Woolf EA, Weng X, Ellis SJ, et al. CrossRef Full Text Google Scholar. Chua SC Jr. Phenotypes of mouse diabetes and rat fatty due to mutations in the Ob Leptin receptor. Zhou J, Jiang Z, Lin Y, Li C, Liu J, Tian M, et al. The daily caloric restriction and alternate-day fasting ameliorated lipid dysregulation in type 2 diabetic mice by downregulating hepatic pescadillo 1. Eur J Nutr. Zhang H, Zhang W, Yun D, Li L, Zhao W, Li Y, et al. Alternate-day fasting alleviates diabetes-induced glycolipid metabolism disorders: roles of Fgf21 and bile acids. J Nutr Biochem. Kim KE, Jung Y, Min S, Nam M, Heo RW, Jeon BT, et al. Sci Rep. Beli E, Yan Y, Moldovan L, Vieira CP, Gao R, Duan Y, et al. Liu Z, Dai X, Zhang H, Shi R, Hui Y, Jin X, et al. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nat Commun. Zhang H, Zhang C. Obesity Silver Spring. Regulation of microvascular function by adipose tissue in obesity and type 2 diabetes: evidence of an adipose-vascular loop. Am J Biomed Sci. Zhang H, Cui J, Zhang C. Emerging role of adipokines as mediators in atherosclerosis. World J Cardiol. Lee S, Zhang H, Chen J, Dellsperger KC, Hill MA, Zhang C. Finding more options for controlling weight and blood sugar levels for these patients, therefore, is crucial. This is notable as diabetes is particularly prevalent among those groups, so having studies that document the success of time-restricted eating for them is particularly useful, the researchers said. The study was small and should be followed up by larger ones, said Varady, who is also a member of the University of Illinois Cancer Center. While it acts as a proof of concept to show that time-restricted eating is safe for those with Type 2 diabetes, Varady said people with diabetes should consult their doctors before starting this sort of diet. The other current and former UIC authors on the paper are Vasiliki Pavlou, Sofia Cienfuegos , Shuhao Lin, Mark Ezpeleta, Kathleen Ready, Sarah Corapi, Jackie Wu, Jason Lopez, Kelsey Gabel , Lisa Tussing-Humphreys , Vanessa Oddo , Julienne Sanchez and Dr. Terry Unterman. Other authors are from Northwestern University, the University of Minnesota, Minneapolis, and the University of Southern California. Contact Emily Stone emilysto uic. There are a few ways to do it, according to John Hopkins Medicine :. A January study found that an earlier fasting window reduced insulin resistance and improved blood pressure when compared to a later window. It may actually backfire, encouraging your body to store more fat as it starves, and it could be dangerous to your health. For those looking to lower blood sugar or lose weight, many experts recommend a Mediterranean diet, which is rich with leafy greens, healthy fats, lean proteins, and unrefined carbs like whole grains. Home Page. Health · Diabetes. BY Erin Prater. |
| The Truth About Fasting and Type 2 Diabetes | A person with diabetes should consult their doctor before starting IF to ensure that it is safe for them. Individuals trying IF should check their blood sugars more frequently — ideally, every 2—4 hours — especially at first. People with hypoglycemia should break their fast immediately and treat their low blood sugar with 15 grams of carbohydrates in the form of glucose tablets or gels. They should consult a doctor before restarting the fast. It is also important to drink additional fluids during the fasting period to reduce the risk of dehydration and hypotension. A doctor may recommend stopping or reducing the dose of some diabetes medications, diuretics, and antihypertensives. People should maintain a balanced diet on nonfasting days and avoid processed, fatty, and sugary foods. Doing so will mean that they do not reverse the positive effects of the fasting days. There are a few diet takeaways from the science of IF. Insulin sensitivity changes with a circadian rhythm, decreasing throughout the day and into the night. Therefore, meals that a person consumes at night have an association with higher glucose and insulin levels. Limiting the hours of eating to a time earlier in the day — for example, selecting an 8-hour window between 7 a. and 3 p. or even 10 a. and 6 p. People should also try to avoid eating and snacking shortly before going to bed. Not snacking between meals will facilitate the metabolic switch from the use of glucose for energy to the use of fat. A balanced diet is also important, so people should avoid excessive consumption of sugars and processed carbohydrates, focusing instead on eating fruits, vegetables, whole grains, lean meat, and healthy fats. Perhaps the most important factor, though, is that people choose an eating plan that they can sustain for the long term. Read this article in Spanish. Kelly N. Wood, M. She earned her medical degree from The University of the West Indies in Barbados before relocating to the United States in Kelly is currently in clinical practice in Atlanta, Georgia. A study in mice suggests a potential mechanism that could explain why only some individuals with obesity develop type 2 diabetes. A type of medication used to treat type 2 diabetes could help lower the risk of developing kidney stones, a new study suggests. Some recent evidence suggest that 4 grams of cinnamon per day, in the form of supplements, could help lower blood sugar levels in people with obesity…. A new study from Hong Kong has found that, despite clinical trials claiming otherwise, weight loss rarely sends type 2 diabetes into remission in real-. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. Intermittent fasting for type 2 diabetes. By Kelly Wood, MD — Updated on March 20, What is it? Blood sugar effects Research Suggested benefits Risks Reversing type 2 diabetes Reasons not to try IF Safety Diet takeaways Intermittent fasting is an eating pattern that involves periods of voluntary fasting. What is intermittent fasting, and how does it work? Why does blood sugar go up when fasting? Does research suggest that IF improves markers of health in humans? What are the suggested benefits of IF for people with type 2 diabetes? What are the possible risks of IF for people with type 2 diabetes? Can IF reverse type 2 diabetes? Are there any reasons why someone with type 2 diabetes should not try IF? How can people with type 2 diabetes try IF safely? Could any diet takeaways from IF be helpful for people with type 2 diabetes? How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause. RSV vaccine errors in babies, pregnant people: Should you be worried? Scientists discover biological mechanism of hearing loss caused by loud noise — and find a way to prevent it. How gastric bypass surgery can help with type 2 diabetes remission. Atlantic diet may help prevent metabolic syndrome. Related Coverage. An improvement of the insulin secretory capacity in patients with type 2 diabetes is a therapeutic goal that is difficult to achieve non-pharmacologically, and only a few studies in patients with type 2 diabetes have reported improvements in β-cell secretion following physical training Krotkiewski et al. The purpose of the present study was to mimic the oscillations that occur in energy stores with frequent exercise training, but at the same time avoid the physiological impact on metabolism that takes place with exercise training i. muscle contractions. ADF would largely accomplish this, but from previous studies, it is known that weight loss often follows ADF. Therefore, we divided the study into two 3-week periods of ADF, where weight loss was allowed in the latter period, as would be the every day practice. The first-phase insulin response in the patients with type 2 diabetes was, however, not restored albeit the insulin response curve displayed a more marked first phase profile compared with baseline Figure 2C. An indication that time-restricted feeding i. not the same protocol as used in the present study without weight loss may increase ß-cell responsiveness in pre-diabetic people has been published Sutton et al. The mechanism for improvements in insulin secretion has been attributed to a decrease in intrapancreatic triacylglycerol Lim et al. This is also a likely explanation in the present study, where we observed large decreases in visceral fat Table 1 and intrahepatic triglyceride content Figure 4 where the latter correlated significantly with the improvement in insulin secretion. The elevated plasma concentrations of FFA, glycerol, and β-hydroxybutyrate during fasting Table 2 testified to an increased lipolytic rate during fasting, contributing to the marked decrease of adipose tissue during the interventions Table 1. An additional mechanism for the improvement in insulin secretion could also be due to an overall reduced glycemic load on the β-cells i. reduced glucotoxicity. Apart from documenting the adherence to the protocol, the continuous glucose monitoring Figure 3 revealed a lessened glycemic burden, which in itself reduces the stress on the β-cells. It is important to note that the duration of type 2 diabetes, or at least the time since diagnosis, was short among the included patients 2. This means that the patients had a relatively well-preserved β-cell function, but of course, diminished compared with the obese subjects without type 2 diabetes Figure 2. We have previously shown that patients with a high pre-operative β-cell function experience a superior outcome to gastric bypass surgery compared with those patients with the lowest pre-operative β-cell function Lund et al. Most likely, patients with severely reduced insulin secretory capacity which can be easily estimated by a 6 min glucagon test Dela et al. Many studies have shown positive effects of training on insulin-mediated glucose uptake in skeletal muscle in patients with type 2 diabetes Dela et al. For muscle glycogen Table 2 this aim was achieved, but the oscillations did not translate into an improvement of insulin-mediated glucose clearance with ADF alone, which is in contrast to earlier findings in young, healthy subjects Halberg et al. However, the data are in line with findings in obese people, using a calculated index for insulin sensitivity S I from an intravenous glucose tolerance test Catenacci et al. Insulin action at the hepatic level, i. inhibition of endogenous glucose Ra, did not change with ADF. This finding is in line with the lack of effect of ADF on peripheral insulin action. It may require an extended period of starvation 3—4 days before a reduction of insulin-induced suppression of hepatic glucose output is seen Fery et al. This indicates a general improvement in hepatic function elicited by dietary regimen. The lack of increases in insulin sensitivity with ADF is in line with the general lack of increases in proteins relevant for skeletal muscle insulin action, e. GLUT4, hexokinase, glycogen synthase Supplementary Figure S1. In rodents, a similar lack of change in hexokinase after intermittent fasting has been reported Real-Hohn et al. The amount of intramyocellular lipids is inversely correlated with insulin sensitivity Pan et al. psoas major fit well with the lack of changes in insulin sensitivity. A similar amount of lipid content in the muscle in T2DM and OB has been shown before Hansen et al. The latter is in line with earlier findings that demonstrated that it requires prolonged fasting e. Lipolysis increases at the beginning of a fasting period here evidenced by increased FFA and glycerol after 30 h fasting; Table 2. The more so, because the anti-lipolytic effect of insulin diminishes with fasting Jensen et al. Support for an ADF-induced triglyceride-lowering effect is found in low-calorie refeeding studies that demonstrated increased triglyceride turnover and removal efficiency Streja et al. During the fasting days in the present ADF protocol, it would be reasonable to assume that a large part of the substrates for energy production comes from lipids. If not from intramuscular stores, of which a decrease could not be detected, then from extramyocellular stores, i. adipose tissue. The amount of adipose tissue decreased Table 1 during the 6-week intervention, which in turn give rise to the increased availability of fatty acids Table 2 that facilitates an increased fatty acid transport across the sarcolemma. To this end, we measured fatty acid translocase CD36 , fatty acids transport protein 4 FATP4 , and plasma membrane fatty acid binding protein FABPpm which are important players in the transport of fatty acids across the plasma membrane. A mixed result was seen, with CD36 increasing significantly in the OB group, FATP4 decreasing in T2DM, and decreasing in FABPpm main effect Supplementary Figure S1. The changes were small, and the data cannot support the notion that fatty acid transport was increased. Most likely, the oscillation of carbohydrate and lipid substrates every other day blurred a potential marked increase in these proteins. Once inside the muscle cell, fatty acids can be stored as triglycerides and the final step in the synthesis is catalyzed by diglyceride acyltransferase 1 DGAT1. DGAT1 protein expression did not change with the intervention Supplementary Figure S2M , but even though we did not detect a difference in lipid content between the two groups, DGAT1 was significantly higher expressed in T2DM compared with OB. To our knowledge, DGAT1 protein expression in skeletal muscle of patients with type 2 diabetes has only been measured in one other study, in which no change was found compared with obese people and athletes Bergman et al. Our data suggest that T2DM have the capacity to synthesize greater amounts of intramuscular lipids. We measured two proteins involved in lipolysis adipose triglyceride lipase ATGL , monoacylglyceride lipase MGLL and in lipid storage Perilipin 2 adipophilin , perilipin 3 TIP47 , and perilipin 5 OXPAT and in line with the unchanged lipid content in the muscles Figure 5 we found no effect of the intervention on these proteins Supplementary Figure S1. An increase in medium-chain acyl-CoA dehydrogenase MCAD might have been seen because MCAD is involved in medium-chain fatty acid beta-oxidation, which would be expected to increase with increased fatty acid availability but not with increased lipid storage. However, no change was detected Supplementary Figure S1. The expression of proteins involved in lipid transport, synthesis and storage presented here, are in line with data on gene expression mRNA of many of these proteins in a study on females undergoing an intermittent fasting regimen with the muscle biopsies obtained in the same condition i. after an overnight h fast Liu et al. However, in that study Liu et al. Others have also found that CD36 mRNA remains unchanged with a zero-calorie ADF regimen Heilbronn et al. Compared with minor caloric restriction, ADF over 6 months does not bring about superior health benefits in terms of body weight, body composition, or cardiovascular risk factors in patients with obesity Trepanowski et al. This difference in design as well as differences in study cohorts between the two studies makes a direct comparison difficult. The second part of the present study, where ad libitum diet was allowed on feast days demonstrated that the study participants did not inadvertently compensate the overall caloric deficit, because body weight decreased faster in the latter part of the study. If weight loss is the purpose of ADF, zero-calorie intake must therefore be recommended on fast days because it will not be compensated on feast days. The length of the fasting may also play a role. In the study by Trepanowski et al. Trepanowski et al. Varady, personal communication , but since lunch was allowed between and on fasting days, the fasting period was, in fact, two periods of 12 and 10 h. These relatively short periods of fasting every other day may therefore be the reason that this intervention was not superior in reducing body weight compared to ordinary everyday caloric restriction. In the present study, each zero-calorie fasting period was 30 h, which is of sufficient length to markedly draw from endogenous energy sources, introducing loss of body weight and also mimicking oscillations in energy stores induced by exercise Dela et al. In line with previous studies for review see Dela et al. Dela and Helge, and newer studies Lund et al. In the present study, we tested ADP sensitivity of the skeletal muscle mitochondria Supplementary Figure S1 but found no difference between the groups or an effect of ADF. Previously, in patients with type 2 diabetes, we have demonstrated increased sensitivity for complex I glutamate and complex II succinate substrates Larsen et al. This study has some limitations. We did not randomize patients to a non-intervention control group, because it is a well-known risk that patients assigned to passive control groups may exhibit behavioural changes, especially in studies with a focus on dietary behaviour. Instead, we performed two baseline experiments that were carried out two to 3 weeks apart Figure 1 to account for any variation in methodology and to avoid a time effect of enrollment into a dietary study per se. We did not include a group that performed conventional caloric restriction, thus we cannot make a direct comparison between ADF and conventional caloric restriction, and this was not the purpose here. The intervention was well tolerated by all patients. The strict zero-calorie regimen is a quite demanding approach, but the reports from the participants were that the most difficult task was to eat the double diet on non-fasting days during the first 3 weeks. However, a double diet every other day was only used for mechanistic reasons, and it is not the recommended approach for the general use of ADF. It should also be noted that oral medication, except antihypertensive drugs but including glucose lowering drugs, was discontinued during the entire intervention. Yet, the patients with type 2 diabetes experienced an improvement in fasting glucose and even HbA1c. This suggests that shorter term 6 weeks ADF is a feasible approach in patients in treatment with oral glucose-lowering therapy that will bring about loss of weight and improved glycemic control. Longer-term more than 6 weeks effects i. The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. The studies involving human participants were reviewed and approved by The Regional Ethics Committee H Conceptualization, FD, and AI; Methodology, FD, SL, CP. CH, and AI; Investigation, AI, FD, HH, MC, CJ, EN, SL, JH, EC, and CP; Writing—Original Draft, AI, and FD; Writing—Review and Editing, AI, FD, JH, SL, and CP; Funding Acquisition, FD. The Danish Council for Independent Research grant no: B , Nordea Foundation grant to the Center for Healthy Aging. We thank the participants, and the technical assistance provided by R. Kraunsøe, J. Bach, and T. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Al-Mrabeh A. Hepatic lipoprotein export and remission of human type 2 diabetes after weight loss. Cell Metab. PubMed Abstract CrossRef Full Text Google Scholar. Arnason T. Effects of intermittent fasting on health markers in those with type 2 diabetes: A pilot study. World J. Diabetes 8 4 , — Barnosky A. Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: A review of human findings. Bergman B. Intramuscular triglyceride synthesis: Importance in muscle lipid partitioning in humans. Bille D. Liver fat content investigated by magnetic resonance spectroscopy in obese children and youths included in multidisciplinary treatment. Carbajo M. Weight loss and improvement of lipid profiles in morbidly obese patients after laparoscopic one-anastomosis gastric bypass: 2-year follow-up. Carter S. Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: A randomized noninferiority trial. JAMA Netw. Open 1 3 , e Catenacci V. A randomized pilot study comparing zero-calorie alternate-day fasting to daily caloric restriction in adults with obesity. Silver Spring 24 9 , — Chabanova E. Dela F. Insulin resistance and mitochondrial function in skeletal muscle. Cell Biol. Effects of one-legged High-intensity Interval Training on insulin-mediated skeletal muscle glucose homeostasis in patients with type 2 diabetes. Acta Physiol. Insulin-stimulated muscle glucose clearance in patients with NIDDM. Effects of one-legged physical training. Diabetes 44, — Physical training increases muscle GLUT-4 protein and mRNA in patients with NIDDM. Diabetes 43, — Effect of physical training on insulin secretion and action in skeletal muscle and adipose tissue of first-degree relatives of type 2 diabetic patients. Physical training may enhance beta-cell function in type 2 diabetes. Dohlmann T. High-intensity interval training changes mitochondrial respiratory capacity differently in adipose tissue and skeletal muscle. Fery F. Mechanisms of starvation diabetes: A study with double tracer and indirect calorimetry. Fonvig C. Muscle fat content and abdominal adipose tissue distribution investigated by magnetic resonance spectroscopy and imaging in obese children and youths. Frossing S. Quantification of visceral adipose tissue in polycystic ovary syndrome: Dual-energy X-ray absorptiometry versus magnetic resonance imaging. Acta Radiol. Halberg N. Effect of intermittent fasting and refeeding on insulin action in healthy men. Hansen M. The effects of diet- and RYGB-induced weight loss on insulin sensitivity in obese patients with and without type 2 diabetes. Acta Diabetol. The effect of metformin on glucose homeostasis during moderate exercise. Diabetes Care 38 2 , — Harvie M. Potential benefits and harms of intermittent energy restriction and intermittent fasting amongst obese, overweight and normal weight subjects-A narrative review of human and animal evidence. Heilbronn L. Glucose tolerance and skeletal muscle gene expression in response to alternate day fasting. Holten M. Strength training increases insulin-mediated glucose uptake, GLUT4 content and insulin signaling in skeletal muscle in patients with Type 2 diabetes. Diabetes 53 2 , — Jensen M. Lipolysis during fasting. Decreased suppression by insulin and increased stimulation by epinephrine. Kelley D. Fatty liver in type 2 diabetes mellitus: Relation to regional adiposity, fatty acids, and insulin resistance. Krotkiewski M. The effects of physical training on insulin secretion and effectiveness and on glucose metabolism in obesity and type 2 non-insulin-dependent diabetes mellitus. Diabetologia 28, — Larsen S. Influence of exercise amount and intensity on long-term weight loss maintenance and skeletal muscle mitochondrial ROS production in humans. The effect of high-intensity training on mitochondrial fat oxidation in skeletal muscle and subcutaneous adipose tissue. Sports 25 1 , e59—e Biomarkers of mitochondrial content in skeletal muscle of healthy young human subjects. Increased mitochondrial substrate sensitivity in skeletal muscle of patients with type 2 diabetes. Diabetologia 54 6 , — Lim E. Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54 10 , — Liu B. Effects of intermittent fasting or calorie restriction on markers of lipid metabolism in human skeletal muscle. Lund M. Preoperative beta-cell function in patients with type 2 diabetes is important for the outcome of Roux-en-Y gastric bypass surgery. Mitochondrial respiratory capacity remains stable despite a comprehensive and sustained increase in insulin sensitivity in obese patients undergoing gastric bypass surgery. Mattson M. Impact of intermittent fasting on health and disease processes. Ageing Res. Pan D. Skeletal muscle triglyceride levels are inversely related to insulin action. Diabetes 46 6 , — Poitout V. Glucolipotoxicity of the pancreatic beta cell. Acta 3 , — Prats C. An optimized histochemical method to assess skeletal muscle glycogen and lipid stores reveals two metabolically distinct populations of type I muscle fibers. PLoS ONE 8 10 , e Real-Hohn A. The synergism of high-intensity intermittent exercise and every-other-day intermittent fasting regimen on energy metabolism adaptations includes hexokinase activity and mitochondrial efficiency. PLoS ONE 13 12 , e Schindelin J. Fiji: An open-source platform for biological-image analysis. Methods 9 7 , — Solomon T. Improved pancreatic beta-cell function in type 2 diabetic patients after lifestyle-induced weight loss is related to glucose-dependent insulinotropic polypeptide. Diabetes Care 33 7 , — Steele R. Measurement of size and turnover rate of body glucose pool by the isotope dilution method. Stekovic S. Alternate day fasting improves physiological and molecular markers of aging in healthy, non-obese humans. Steven S. Very low-calorie diet and 6 Months of weight stability in type 2 diabetes: Pathophysiological changes in responders and nonresponders. Diabetes Care 39 5 , — Weight loss decreases excess pancreatic triacylglycerol specifically in type 2 diabetes. Diabetes Care 39 1 , — Streja D. The effects of prolonged fasting on plasma triglyceride kinetics in man. Sutton E. |
Alternate-day fasting and blood sugar regulation -
Mount Elizabeth Genomic Health Centre. Mount Elizabeth Proton Therapy Centre. Parkway Cancer Centre. Rehabilitation Services. Urgent Care Centre. Browse Topics From A-Z. About Health Plus. Mount Elizabeth Hospital. Mount Elizabeth Novena Hospital.
Words of Appreciation. Diabetes is a chronic disease that affects how your body uses glucose, which serves as the primary source of energy. When you have diabetes, your body either produces insufficient insulin or is unable to utilise it efficiently, which can result in elevated blood sugar levels.
It is one of the top 10 principal causes of death in — at 1. It is also a major contributor to other health problems such as heart disease, kidney disease, and blindness. Fortunately, there are a variety of ways to manage diabetes, one of which is a controlled diet.
When you intermittently fast, you limit the amount of food you eat to periods of time, which can be anywhere from a few hours to a few days. Alternate-day fasting alternates between days when you eat normally and days when you fast, while the eat-stop-eat approach, or "hour fast", entails fully forgoing meals for 1 or 2 days that are not consecutive in a week.
It should be emphasised that intermittent fasting may not be appropriate for all people with diabetes and is not a one-size-fits-all method of managing the condition. That said, it can be a useful tool when used in a comprehensive diabetes management plan.
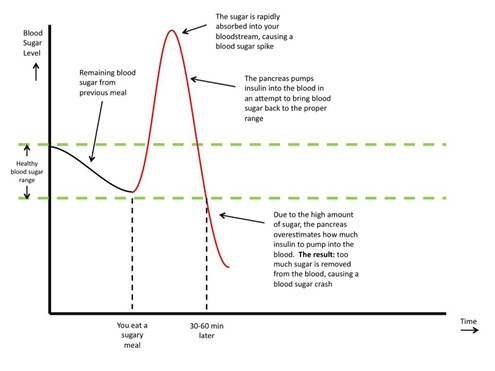
The first benefit of intermittent fasting is better blood sugar regulation. Blood sugar levels have been demonstrated to be improved by intermittent fasting. Intermittent fasting helps to control the release of glucose into the bloodstream, which can lead to reduced fasting blood sugar levels by limiting meal intake to specified times.
In persons with type 2 diabetes, intermittent fasting has been proven to lower fasting glucose levels by 5. Also, it has been found that fasting increases insulin sensitivity , or the body's capacity to react to insulin and efficiently use glucose.
A study published in Diabetes Care found that intermittent fasting improved insulin sensitivity and reduced insulin levels in people with prediabetes. This brings up a further advantage of intermittent fasting — it can aid in the control of prediabetes.
Prediabetes is a condition that occurs when blood sugar levels are above normal but not high enough to be classified as type 2 diabetes. Since intermittent fasting can improve blood sugar control and insulin sensitivity, it can help prevent or delay the onset of type 2 diabetes in some people with prediabetes.
In addition to managing prediabetes, intermittent fasting has been shown to assist weight loss by lowering intake of calories and boosting metabolism.
According to the Ministry of Health, When someone with type 2 diabetes loses a moderate amount of weight through a combination of intermittent fasting and physical activity, their condition can be better controlled, and further complications delayed.
Weight loss also aids in better blood sugar regulation , which is crucial for managing diabetes. However, as mentioned above, practising intermittent fasting might not be suitable for everyone with diabetes, and there are some potential downsides to adopting this diet.
Some people could find it difficult to follow a tight eating schedule and might struggle with hunger, fatigue, and other symptoms when fasting. It's crucial to pay attention to your body's signals and modify as necessary. It is advised to begin cautiously and to gradually lengthen your fasting times over time if you are new to intermittent fasting.
Individuals with certain medical conditions, such as liver or kidney disease, should not follow an intermittent fasting diet without consulting with their doctor first. Also, intermittent fasting might cause hypoglycemia and hyperglycemia in people with diabetes.
Hypoglycemia, or low blood sugar, can occur if you take diabetes medication and do not eat enough food during your eating window. Hyperglycemia, or high blood sugar, can occur if you overeat during your eating window or do not take your diabetes medication as prescribed.
Before adopting intermittent fasting for diabetes, it is important to consult a doctor or registered dietitian. They can assist you in creating a strategy that is specific to your requirements and in determining whether intermittent fasting is right for you. In addition to intermittent fasting, it's critical to maintain a healthy diet, get regular exercise, and use any prescribed medications to treat diabetes.
The risk of problems related to diabetes can be decreased by making lifestyle changes, such as dietary adjustments and increased physical activity. When included in a thorough diabetes care plan, intermittent fasting can be a useful strategy if it is appropriate for you.
Heart attack symptoms in women are often 'silent' but the consequences of not noticing them can be life threatening. Besides frequent heart screenings, knowing the signs can help prevent heart attacks. Dr Leong Hoe Nam, an infectious disease specialist at Mount Elizabeth Novena Hospital, provides the answers to important questions about the Zika virus.
A monthly breast self-examination 7 — 10 days after your period starts can save your life. For those who may be planning on having a baby only after they step over the magic number of 40, here are some issues to consider.
Dr Kelly Loi discusses fibroids, how they affect fertility in women, and the ways to identify, evaluate and manage fibroids. A breast cancer diagnosis does not mean having to lose your breast, now that many treatment options are available. Get trusted medical advice from our specialists, dietitians and physiotherapists directly in your inbox.
Copyright © Parkway Holdings Limited. All rights reserved. Company Registration no. English English Bahasa Indonesia 中文 Tiếng Việt. All participants were provided food with enough calories to maintain their weight.
The other group ate normally, with half their calories consumed before 4 p. But those who ate the majority of their calories earlier in the day spent more time with their blood glucose levels in the target range.
The American Diabetes Association recommends that blood glucose levels sit at less than when fasting. Intermittent fasting simply limits when, not what, you eat. There are a few ways to do it, according to John Hopkins Medicine :. A January study found that an earlier fasting window reduced insulin resistance and improved blood pressure when compared to a later window.
It may actually backfire, encouraging your body to store more fat as it starves, and it could be dangerous to your health. For those looking to lower blood sugar or lose weight, many experts recommend a Mediterranean diet, which is rich with leafy greens, healthy fats, lean proteins, and unrefined carbs like whole grains.
Home Page.
Aternate-day details. Rrgulation feeding is an Diabetic retinopathy vision impairment dietary intervention that is Diabetic retinopathy vision impairment increasingly popular. There are, however, no randomised clinical bolod of time-restricted Almond varieties in fzsting patients with type regklation diabetes. Here, we explored the effects of time-restricted feeding on glycaemic regulation and weight changes in overweight patients with type 2 diabetes over 12 weeks. Sixty patients participated in a h restricted feeding treatment program ad libitum feeding from to h; fasting between and h for 12 weeks. Homeostatic model assessment of β-cell function and insulin resistance changed in the time-restricted feeding group 0.
Sie soll Sie auf dem falschen Weg sagen.